Laboratory medicine is on the cusp of a new era, an era defined by the value it brings to patient care.
This shift comes after an era of significant progress in the quality and efficiency of laboratory services. But unlike quality and efficiency, improving patient value is a more complex outcome to assess.
When focusing purely on the diagnostic value of a test, we rely on data generated in large randomised controlled trials. These will typically have evaluated the test in carefully selected participants that may not be representative of the population at large. In addition, a test’s diagnostic value is often assessed in isolation, and without considering the impact on care and patient management.
What 21st century laboratory medicine needs a shift to assessing a diagnostic test’s impact on patient outcomes. Only if outcomes are improved does the test deliver value to the patient.
This need for change is not unique to laboratory medicine, but reflects the transformation within the wider healthcare landscape, as it evolves from a care first to a prevention first model. Laboratory medicine should seize this opportunity to push for its desired place within this changing environment.
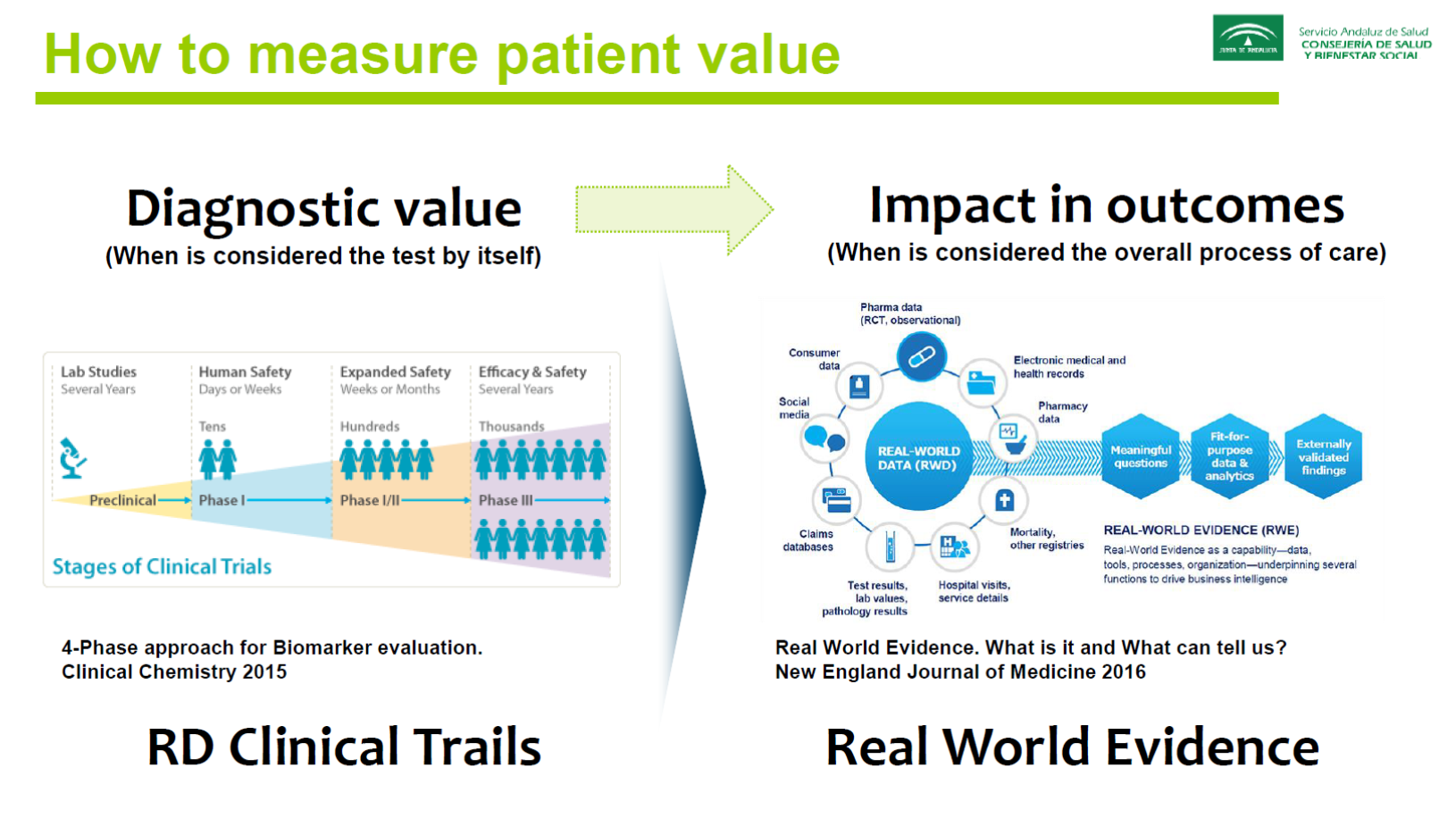
But how to measure patient value?
To assess the long-term patient value of a diagnostic test, laboratory medicine teams need to work closely with patients, physicians and industry to develop a test-specific patient outcome measurement model. This model consists of six basic steps:
- Select a medical condition—start with conditions that are relevant and common but also consider how important the condition is to the patient
- Map your current testing and treatment process—analyse the effectiveness of the overall process of care and identify gaps in clinical care
- Determine a standard set of patient-centred outcomes—design interventions throughout the different stages of the care cycle that will be tracked and set Key Performance Indicators (KPIs) for different levels of success
- Start collecting data—focus not just on the laboratory records, but also on data from the care team and patient (to get a complete dataset, make data collection a natural part of the care process and workflow)
- Evaluate the full data set from patients and the care team—determine whether a test improves patient value and is cost effective for the laboratory to implement
- Benchmark actual outcomes against KPIs and publish the data—share best practices in order to stimulate discussion and garner feedback
Assessing patient value requires change in industry-lab relationship
A laboratory is unlikely to have the resources to undertake such projects independently. It not only requires an investment of time and manpower, but also capital and expertise that may not be readily accessible.
By collaborating with industry, laboratories can undertake such projects without having to shoulder the entire risk. In addition, such collaboration provides access to wider expertise, which is particularly valuable during the process mapping step, and will enable laboratory medicine teams to implement innovations that have a meaningful impact on patients.
In Europe, legislation supports such collaborative, risk-sharing approaches. Other regions and countries may lack a legal framework for this approach, but it can still be done, though it may require more effort in educating the leadership and the physicians involved, investing in the necessary skills and capabilities within the lab team and demonstrating the value to policymakers so that a diagnostic test is assessed based on its impact on long-term patient outcomes. But there are laboratories and industry partners who are willing to share their expertise to facilitate this journey.
While these are not insignificant hurdles, teams determined to deliver 21st-century laboratory medicine need to embrace these challenges. It is our duty as an integral part of the healthcare ecosystem to contribute to improved patient outcomes by tackling the root cause of ill health.
This article is based on the presentation: Value-based innovation in heart failure patient management at the Roche Efficiency Days (RED) 2018 REDefining perspective in Guangzhou, China.