Sepsis is a global killer. About 27 million people around the world develop sepsis every year, and some eight million people die from it, according to a November 2018 article in The Lancet [1]. This leaves 19 million people living with the long-term consequences of the infection. In Thailand alone, this translates to 175,000 infections with sepsis per year and some 45,000 deaths. This mortality rate is higher than the combined mortality rate of acute ST-elevated MI and stroke. Many of these deaths can be prevented with early detection and diagnosis.
The Thai Ministry of Public Health made a commitment in its 2019 Strategic Plan to cut sepsis-related mortality to less than 22 per cent by 2022, with an interim target of less than 30 per cent by 2018. However, current rates continue to exceed even the interim target, with severe community-acquired sepsis mortality rates hovering at around 32 per cent.
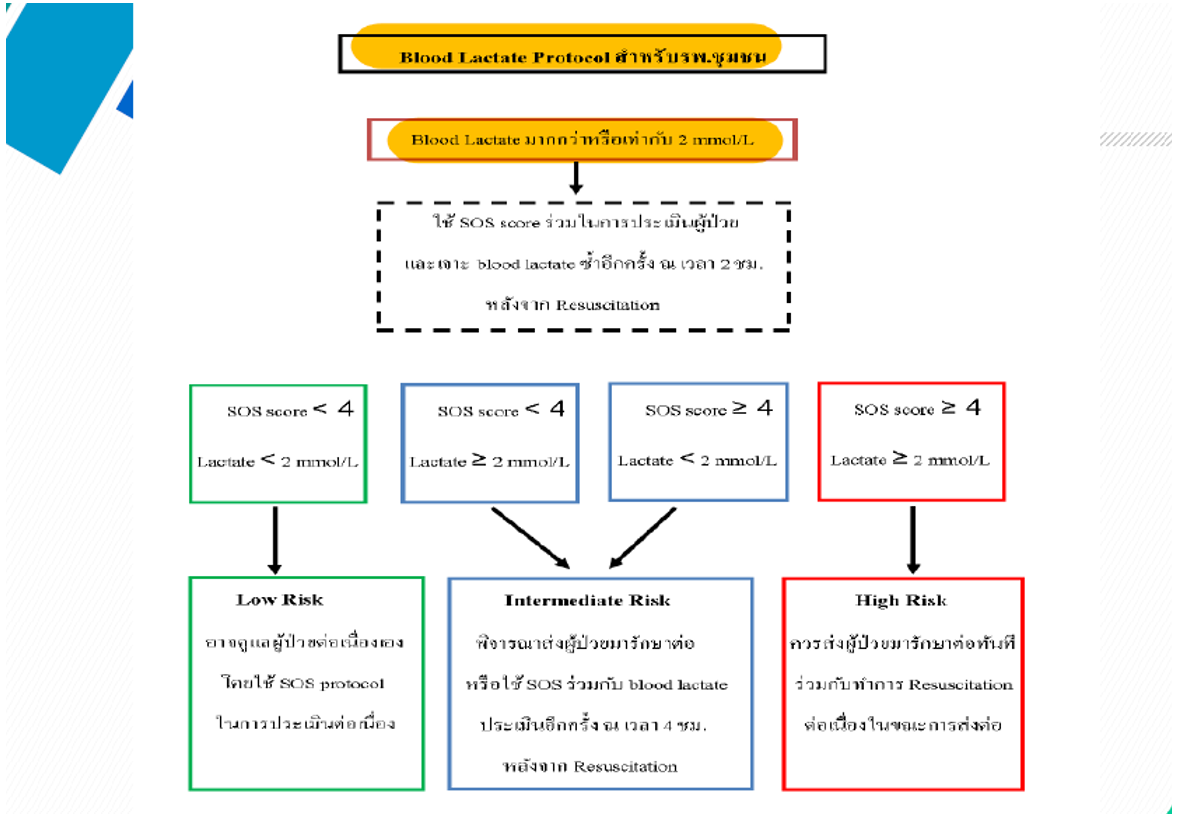
To achieve the Ministry’s goals and improve care for patients, hospitals have to promote diagnostic parameters that will allow practitioners to make accurate and early diagnoses of sepsis and septic shock. Reviewing existing guidelines, the Thai Society for Critical Care Medicine recommended that the following two parameters be included as early screening for sepsis: (a) search out severity (SOS) score of four or more; and (b) lactate levels of ≥2mmol/L.
Based on these recommendations, the sepsis care team at Phitsanulok Hospital developed a new protocol that stratifies patients first based on their blood lactate levels and then their SOS score. Any patient with an SOS score of more than four was deemed at high risk of sepsis.
As studies have shown that lactate levels can be accurately detected in venous, arterial and capillary blood [2], we decided to incorporate a point–of–care (POC) testing service located in the community hospitals in our network.
These hand–held POC devices return results in just one minute. This is significantly faster than can be achieved by traditional laboratory–based services.
Some studies have found that these POC devices may be less accurate than traditional lab-based analysis [3]. Our monitoring of 13 hospitals that use the POC device has determined that the blood lactate scores are within an acceptable range, and so with these devices, the benefits of a faster sepsis diagnosis can be achieved.
After implementing our new local protocol, the mortality rate among patients with sepsis was just over 27 per cent, coming in significantly below the interim target of less than 30 per cent. With a wider roll-out of protocols like this, we can avoid unnecessary deaths from this infection and make progress towards meeting the ambitious national target of a mortality rate of less than 22 per cent by 2022.
Sepsis can be treated when diagnosed early. Incorporating the latest POC testing capabilities into our laboratory medicine processes offers patients better outcomes and reduces the burden on the healthcare system.
[1] Gilbert, A,J. 2018. Sepsis care bundles: a work in progress. The Lancet, 6(11), pp.821-823.
[2] Pattharanitima, P., et al., 2011. Correlation of arterial, central venous and capillary lactate levels in septic shock patients. Journal of the Medical Association of Thailand, 94 supplementary 1, S175-180.
[3] Stoll, D., et al., 2018. Capillary and venous lactate measurements with a handheld device compared to venous blood-gas analysis for emergency patients. Scandinavian journal of trauma, resuscitation and emergency medicine, 26(1), pp.47.