In the ongoing fight against the COVID-19 pandemic, many healthcare systems are adding interleukin-6 (IL-6) to their diagnostic toolkit. An early predictor of severe COVID-19, IL-6 is an ideal prognostic biomarker because it can be detected from an easily accessible biological source (serum or plasma) and via well-characterised, rapid assay systems. A growing body of evidence highlights its potential in becoming an integral part of critical COVID-19 management [1].
In a recent webinar hosted by Roche Diagnostics, Dr Conrad Liles, Professor and Associate Chair of Medicine in the University of Washington Department of Global Health, and Dr Tobias Weinberger, Senior Physician at Ludwig Maximilian University Hospital, discussed the role of IL-6 as a biomarker in COVID-19 management. The webinar focused on clinical research and case sharing from the United States and Germany, but it offers insights that have relevance for many healthcare systems in Asia Pacific—particularly those facing high caseloads of severe and critically ill patients.
An early predictor of respiratory failure
IL-6 is a pleiotropic inflammatory cytokine and a major component of the cytokine storm in patients with severe COVID-19. Increased serum or plasma IL-6 is the most reported cytokine abnormality in patients with COVID-19 [2]. Several studies in Chinese populations have also found that elevated IL-6 is associated with poorer outcomes and higher fatality [3-5]. As lung macrophages express a higher level of IL-6 compared with blood monocytes, Dr Weinberger noted that “IL-6 may represent a window into the lung and could be a good diagnostic tool to address disease severity”.
A prospective cohort study by Dr Weinberger’s research group found that elevated IL-6 was highly predictive of the need for mechanical ventilation in 89 hospitalised COVID-19 patients at Ludwig Maximilian University Hospital [6]. Maximal IL-6 level before intubation at a cut-off point of 80pg/ml showed the strongest association with positive and negative predictive values of 74% and 83%, respectively. In the combined cohort, IL-6 predicted the need for intubation up to 23.2 hours before the patient received it.
Despite the predictive value of maximal IL-6 in the study, Dr Weinberger generally recommends IL-6 testing at initial assessment as they also found that IL-6 retained high sensitivity in detecting patients at risk of respiratory failure at a low cut-off threshold of 35pg/ml.
At the University of Washington Medical Center, IL-6 is measured in hospitalised patients who show signs of clinical deterioration such as hypoxia but are not intubated or in ICU. “Our approach is to treat the individuals to mitigate the need for mechanical ventilation and stop progression of lung disease…to prevent acute lung injury in individuals who have acute hypoxemic respiratory failure due to COVID prior to intubation,” Dr Liles shared.
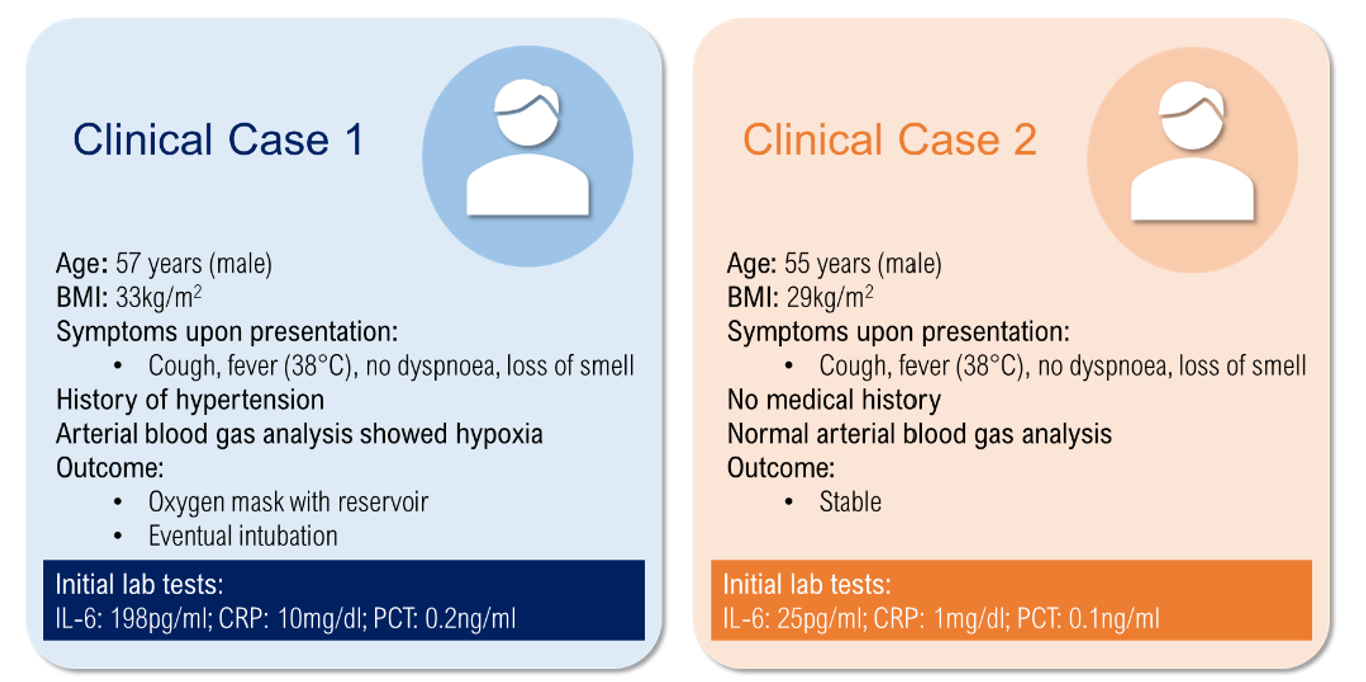
Dr Weinberger emphasised the difficulty in assessing the prognosis of COVID-19 patients due to a broad spectrum of disease courses and silent hypoxia. He presented two patient cases with similar symptoms, one of whom experienced rapid clinical deterioration within two days and required eventual intubation (Figure 1). Here, he reiterated that a laboratory parameter such as IL-6 is useful to identify the need for ventilatory support in patients with silent hypoxia.
Growing interest in IL-6 in Asia Pacific
In the Asia Pacific region, the utility of IL-6 as a biomarker for COVID-19 management is being actively explored in China, where it is specifically mentioned in the Chinese Clinical Guidance for COVID-19 Pneumonia Diagnosis (7th edition) as an indicator of severe and critical cases in adults [7]. Clinical stakeholders in India and other countries are also taking interest.
As an early predictor of respiratory failure compared with other inflammatory biomarkers such as ferritin and C-reactive protein, IL-6 can help identify critical patients in a more timely and effective manner so that physicians can organise intensive care or intensify treatment as appropriate. In this respect, assessment of IL-6 may be of particular benefit in Asian countries which are experiencing high ICU bed occupancy and mortality rates such as Indonesia [8].
Want to learn more about the role of IL-6 in COVID-19 management? Click here to watch the recording of the webinar.
References:
[1] Del Valle DM, Kim-Schulze S, Huang H-H, et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat Med. Published online August 24, 2020:1-8.
[2] Ragab D, Salah Eldin H, Taeimah M, Khattab R, Salem R. The COVID-19 Cytokine Storm; What We Know So Far. Front Immunol. 2020;11.
[3] Liu Z, Li J, Chen D, et al. Dynamic Interleukin-6 Level Changes as a Prognostic Indicator in Patients With COVID-19. Front Pharmacol. 2020;11.
[4] Chen X, Zhao B, Qu Y, et al. Detectable Serum Severe Acute Respiratory Syndrome Coronavirus 2 Viral Load (RNAemia) Is Closely Correlated With Drastically Elevated Interleukin 6 Level in Critically Ill Patients With Coronavirus Disease 2019. Clin Infect Dis.
[5] Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846-848.
[6] Herold T, Jurinovic V, Arnreich C, et al. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J Allergy Clin Immunol. 2020;146(1):128-136.e4.
[7] Chinese Clinical Guidance for COVID-19 Pneumonia Diagnosis and Treatment (7th edition) 抗击新冠肺炎. Accessed August 10, 2020. http://kjfy.meetingchina.org/msite/news/show/cn/3337.html
[8] Jakarta’s Covid-19 Response Team. Jakarta’s Covid-19 Response Team. Accessed August 25, 2020. https://corona.jakarta.go.id/en









